Following close on the heels of the COVID -19 vaccination programme a new global initiative is being developed to address the urgency of the TB PANDEMIC. This however poses an important question:
Why are 80% of South Africans infected with TB after a BCG vaccination programme of over 70 years?
Appreciating the urgency and scale of the TB problem and in response to the initiatives of the Centre for Tuberculosis Research Johns Hopkins University, the US National Institutes of Health, Centres for Disease Control and Prevention, Food and Drug Administration, the Bill and Melinda Gates Foundation, Unitaid, USAID, and several small foundations and partners: The National Research Foundation, eight universities, including the Cape Peninsula University of Technology, Rhodes University, Stellenbosch University and the Universities of Cape Town, Johannesburg, Kwa-Zulu Natal, Pretoria, and South Africa, the Universities of the Witwatersrand and Western Cape, the African Population and Health Research Centre and the Nigerian Academy of Science to develop a new TB vaccine:
It is essential to first take cognisance of what science and research has documented on the subject:
SUMMARY:
In the context of the ZAGHOUANI study (PMC2787701) Zaghouani H1, Hoeman CM, Adkins B Trends in Immunology, 19 Oct 2009, 30(12):585-591 DOI: 10.1016/j.it.2009.09.002 PMID: 19846341 it is evident that the primary cause of the current high incidence of TB in populations is the vaccination of infants at birth.
The further development and implementation of Tuberculosis vaccine programmes can therefore only create further dysfunction and skewing of the adaptive immune response towards Th2 and deplete Th1 CD4 cells.
Given this scenario the probability that populations will face a pandemic of leprosy is highly possible in the future.
The incidence of leprosy is currently held in check with the use of antibiotics.
As more strains of bacteria are becoming resistant through the overuse and misuse of antibiotics it is a matter of time before people are faced with more severe pandemics than the current COVID -19 problem.
The high rates of antimicrobial agent usage in COVID-19 patients are now being blamed for a rapid rise in multidrug-resistant organisms (MDROs), including:
- Extended-spectrum β-lactamase (ESBL)-producing Klebsiella pneumoniae.
- Carbapenem-resistant New Delhi metallo-β-lactamase (NDM)-producing Enterobacterales.
- Acinetobacter baumannii.
- Methicillin-resistant Staphylococcus aureus (MRSA)
- Pan-echinocandin-resistant Candida glabrata.
- Multitriazole-resistant Aspergillus fumigatus.
Experiments by Sir Peter Medawar’s group in the 1950s demonstrated that neonatal exposure to antigen (Ag) (via vaccination) leads to a lack of responsiveness to the same Ag during later encounter.
As most people have received a regimen of vaccinations from infancy the further implementation of vaccine campaigns runs the probable risk of skewing their immune systems, and creating a series of problems far more serious than those that are manifest at the present time.
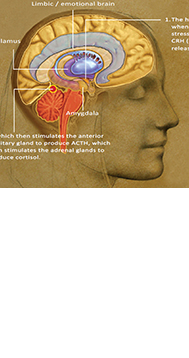
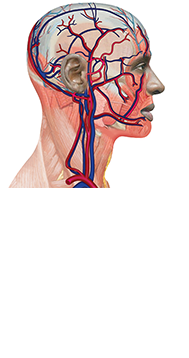
The consequence of stimulating a neonate’s immune system prematurely is an underdeveloped – mutated receptor on the Th1 cell membrane. (An epigenetically hypo-methylated area on the surface of the Th1 cells.)
The immune response in effect becomes tolerogenic instead of immunogenic and skews the response to T helper 2 cells. Interleukin IL-4 then performs apoptosis (kills) the T helper 1 cells.
Th1 cells play important roles in the identification and eradication of intracellular pathogens such as viruses and bacteria, including Mycobacterium tuberculosis, Mycobacterium leprae ( leprosy), and Leishmania.
It is therefore of vital importance that the public, pharmaceutical industry, government and health care clinics take note of the scientific research and adjust their vaccination programmes to exclude infants (under 9 months) from all vaccination programmes.
Note: the Zaghouani study is not the only paper to identify the phenomena of actively acquired tolerance as the exact inverse of ‘actively acquired immunity,’ in vaccinated neonates.
- Actively acquired tolerance of foreign cells. Billingham RE, et al. Nature 1953;172:603–606. [PubMed:13099277]
- Prescott S, et al. Development of allergen-specific T-cell memory in atopic and normal children. Lancet. 1999;353:196–200.
- Induction of Th1 and Th2 immunity in neonatal mice. Science 1996;271:1728– 1730. Forsthuber T, et al. [PubMed: 8596934]
- Enhanced type 2 and diminished type 1 cytokines in neonatal tolerance. Chen N, Field EH Transplantation 1995;59:933–941. [PubMed: 7535960]
- Singh RR, et al. Neonatal peptide exposure can prime T cells and upon subsequent immunization,induce their immune deviation: implications for antibody vs. T cell-mediated autoimmunity. J Exp Med 1996;183:1613–1621. [PubMed: 8666919]
- Powell TJ, Streilein JW. Neonatal tolerance induction by class II alloantigens activates IL-4-secreting,tolerogen-responsive T cells. J Immunol 1990;144:854–859. [PubMed: 2136901]
- Neonatal tolerant immunity for vaccination against autoimmunity. Min B, et al. Intern Rev Immunol 2000;19:247–264.
- Exclusive Th2 primary effector function in spleens but mixed Th1/Th2 function in lymph nodes of murine neonates. Adkins B, et al. J Immunol 2000;164:2347–2353. [PubMed: 10679069]
- Delayed maturation of an IL-12 – producing dendritic cell subset explains the early Th2 bias in neonatal immunity. Hyun-Hee Lee , Christine M. Hoeman , John C. Hardaway , F. Betul Guloglu , Jason S. Ellis , 1 Renu Jain , Rohit Divekar , Danielle M. Tartar , Cara L. Haymaker , and Habib Zaghouani.
- The Primary Responses of Murine Neonatal Lymph Node CD41 Cells are Th2-skewed and are Sufficient for the Development of Th2-biased Memory BECKY ADKINS, YURONG BU, VLADIMIR VINCEK and PATRICIA GUEVARA Department of Microbiology and Immunology, University of Miami Medical School, Miami, FL 33136, USA; Department of Pathology, University of Miami Medical School, Miami, FL 33136, USA.

Copyright 2022 | Craniosacral art c.c. 200808992923